Understanding Low Testosterone in Military Veterans
Take Action for Better Health
Discover the impact of low testosterone on the lives of our veterans and learn how you can address low testosterone levels.
The Importance of Addressing Low Testosterone in Veterans
Low testosterone is becoming a growing concern if you’re a military veteran. You have made countless sacrifices to serve your country and have faced numerous challenges and obstacles along the way. Unfortunately, many veterans face new health issues after leaving active duty, including low testosterone.
When I enlisted, I didn’t consider my long-term health as important. I was 19 and just wanted to send it for Canada (and hopefully get a girlfriend for my service). I’m now a middle aged, tired, low T, degenerative disc diseased veteran that wants to help educate my fellow brothers and sisters in arms. Thankfully, I did at least get that girlfriend and we now have two beautiful children.
I contend there’s a massive, underlying issue that is contributing to more veterans committing suicide and nobody is paying enough attention to it – low testosterone.

Percentage of Men Suffering from Low Testosterone After Age 45.
Percentage of Male Veterans Reporting Mental Health Issues

Percentage of Veterans Diagnosed With Insomnia

Percentage of GWOT Veterans Exposed to Burn Pit Toxicity
What Is Low Testosterone?
Low testosterone, also known as hypogonadism, is a medical condition that affects the production of the male sex hormone, testosterone. Testosterone plays a critical role in maintaining muscle mass, bone density, and sex drive. Unfortunately, low testosterone is becoming an increasingly common problem among military veterans. However, there is still no definitive study showing the absolute rates of low testosterone in the military population; anecdotally, there seems to be substantial evidence piling up.
Here’s my argument.
Since the start of the Global War on Terror (GWoT), the operational tempo and demands on the all volunteer militaries from all NATO countries was extreme. The wars raged for nearly twenty years with many soldiers serving multiple deployments. This doesn’t include the near constant training cycle when back home and the inability for many soldiers to recover physically and emotionally between deployments.
Because of these very high stress demands, soldiers were exposed to ungodly levels of sleep deprivation, toxic exposure, mild traumatic brain injuries and emotional stress. The combination of each of these factors, seems to have led to endocrine system ruin for a lot of veterans.
Let’s start with the basics of human biology to get a better understanding of the problem.
The HPG Axis
It’s important to understand what is going on. We have a clever cascade of hormones that starts in the brain to initiate the synthesis of testosterone in the testes. Scientists call this the “Hypothalamus, Pituitary, Gonadal Axis”.
The hypothalamus, a small structure inside your brain, secretes a hormone called Gonadotropin-releasing hormone (GnRH) which then stimulates the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). LH then drives the production of testosterone in the testes.
In a conversation I had with Dr. Machen, co-author of the study, “Direct conversion from long‐acting testosterone replacement therapy to Natesto allows for spermatogenesis resumption: Proof of concept”, he explains the importance of determining what’s causing your hypogonadism (low T). Any misfiring of the cascade of hormones in the HPG axis will have an effect on your testosterone production.
What’s important to remember is that once your natural testosterone production has fallen significantly or below the “normal” range of approximately 300ng/dl of free testosterone, it’s very hard to get it much higher without exogenous testosterone replacement. However, ask Dr. Machin explains, you can naturally increase your free testosterone levels with some lifestyle changes such as:
- Losing body fat
- Lifting heavy weights
- Eating a balanced diet free of crap
- Getting more vitamin D
- Improving your sleep
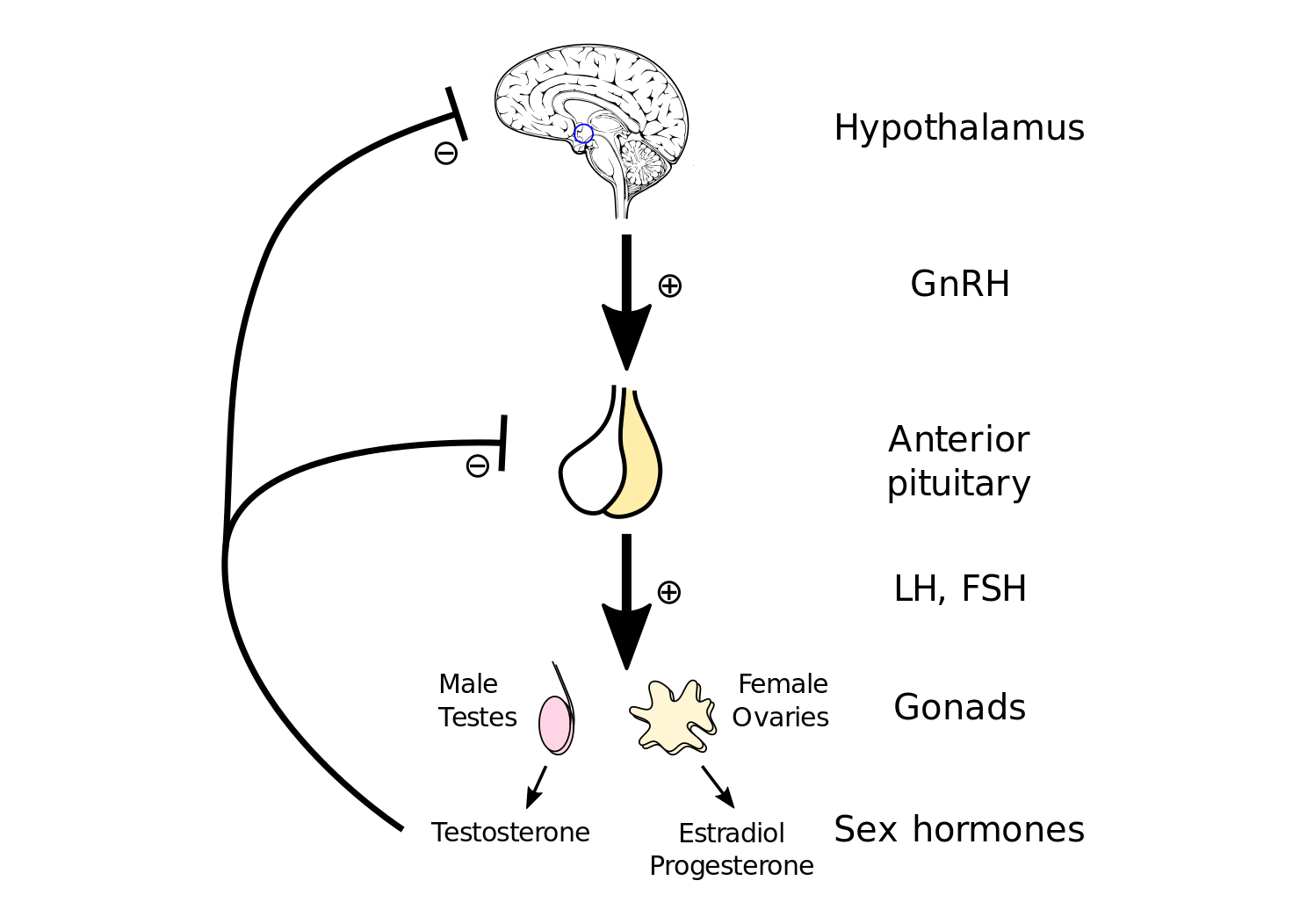
HPG Axis
Sleep Deprivation
Of important note, there is plenty of evidence that poor sleep affects the proper functioning of the hypothalamus which I explain in more detail here. I had a great podcast about poor sleep with Navy SEAL, Dr. Kirk Parsley.
As I mentioned earlier, sleep can play a massive role in your testosterone levels. As Dr. Parsley mentioned, a poor night’s sleep will cut your free testosterone by 30%. Additionally, deployed soldiers are more prone to consuming copious amounts of Ambien to accommodate for the irregular sleep patterns due to night raids, mortar attacks and late night Wii tennis tournaments. The net effect of Ambien is negative according to Dr. Parsley who worked closely with his Navy Seals on this issue.
In a landmark study in the journal, Nature, it was discovered that 50% of the American army was prescribed a narcotic sleep aid for chronic insomnia.
What does this mean for you?
If you’re a veteran, you likely destroyed your sleep habit. I believe this is likely the main cause of falling testosterone levels that are outpacing the civilian drop in testosterone levels. It was shown that Rangers getting out of the field after their 8 week course had an 80% reduction in testosterone levels!
Interestingly, 55% of male soldiers and veterans from Fort Bragg tested having low vitamin D concentrations. Of those with lowest vitamin D levels, significantly lower testosterone concentrations were observed, especially for those who were younger and with a higher BMI. It’s known that vitamin D acts on the HPG axis that can dysregulate GnRH activity and effects your circadian rhythm required for optimal sleep.

Toxic Exposure
If you’re a Canadian veteran this will likely be earth shattering news for you but for my American brothers and sisters, this is old news. Everyone that deployed to Iraq or Afghanistan has been exposed to high levels of environmental toxins. These toxins include furans, PCBs, heavy metals and the list goes on and on. Because of this high level of exposure, Congress passed the Pact Act in the United States that is a law that expands VA health care and benefits for Veterans exposed to burn pits, Agent Orange, and other toxic substances.
Exposure to burn pits is a disaster for your endocrine system. One of the “forever chemicals” released from burn pits are polyfluoroalkyl substances (PFAS). These chemicals are used in fire-resistant gear and a host of other military gear. One of the most worrying effects of PFAS is their effect on Leydig cells in the rat testis, causing Leydig cell hyperplasia and lower testosterone levels, similar to clinical observations in infertile men.
The half lives of these chemicals range from 2 to 35 years! Meaning they reduce their concentration in your cells by half every 2 to 35 years, giving them their name, “forever chemicals”.
I chatted with Gruntstyle Chief Brand Officer, Tim Jensen, about impacts of toxic exposure due to burn pits.
Mild Traumatic Brain Injury
If you were in a combat arms trade in the military, the odds of you having been exposed to mild traumatic brain injury is high. Estimates vary but the rate of mTBI in the military is anywhere between 5%-35% with the majority of these exposures due to blast waves. This includes blasts endured during training and combat. Considering that repeated exposure to a grenade range as an RSO can result in an mTBI, you can see how prevalent this issue may be.
An mTBI affects the HPG axis we discussed earlier. It interferes with the gonadotropins LH and FSH and by extension, affects testosterone production. After 12 months post mTBI, 15% of patients in a recent study, had not fully recovered. The repeated exposures in the military means you could easily compound an mTBI into a serious neurological issue if you don’t take the time to heal.

Emotional Stress
Chronically high levels of the stress hormone, cortisol, can have a detrimental effect on your testosterone levels. Cortisol is crucial to keeping us alive and well when in balance with regular hormonal function and metabolism. It’s responsible for flooding the bloodstream with glucose in a time of fight or flight, for example. In the veteran world, emotional stress which can include:
- Your wife emptying your house and changing the locks when you come home from deployment;
- A posting to Shilo, Manitoba;
- Having the VA cut your disability award in half; and
- Losing a battle buddy
We’ve lived through a lot of stressful situations and my favorite expression is, “the body keeps the score.” So, you may think that the awful stuff that’s happened to you is nothing to worry about. You may be right, and you may rationalize it away, but has it been dealt with appropriately. If not, it may be crushing your endocrine system and destroying your testosterone levels.

Symptoms Of Low Testosterone
Symptoms of low testosterone can range from mild to severe and may include decreased energy levels, decreased sex drive, erectile dysfunction, mood changes, and decreased muscle mass. In severe cases, low testosterone can lead to other health problems, such as osteoporosis, decreased bone density, and an increased risk of heart disease.
Diagnosing low testosterone starts with a simple blood test to measure testosterone levels. If the levels are found to be low, further tests may be conducted to determine the underlying cause. Depending on the cause, treatment options may include testosterone replacement therapy, lifestyle changes, or a combination of both. According to a study published in the Journal of Clinical Endocrinology & Metabolism, military veterans treated with testosterone replacement therapy had a significant all cause mortality reduction.
Testosterone Replacement Therapy
Testosterone replacement therapy can be delivered in various forms, including injections, skin patches, gels, or pellets. According to a study published in the New England Journal of Medicine, testosterone replacement therapy has been shown to effectively increase testosterone levels and improve symptoms in most cases. However, it is important to note that testosterone replacement therapy does come with certain risks. In some cases, testosterone replacement therapy has been linked to an increased risk of heart disease, stroke, and prostate cancer. Before starting any form of testosterone replacement therapy, it is crucial to discuss the risks and benefits with your doctor.
Recently, a new testosterone therapy has entered the market called Natesto®. This is a novel, FDA approved nasal gel that is showing some great results. A recent study showed that replacing long-acting testosterone therapy with short acting testosterone therapy, like Natesto, spermatogenesis is maintained in some men. This is really important if you’re a young buck that still has a desire to have a few more children.
I chatted in depth with Dr. Luke Machen about testosterone replacement therapy. CLICK HERE to listen to our conversation.
Dr. Peter Attia in his conversation with Derek from, More Plates More Dates, has also made a compelling case for Natesto for its reduction of hematopoiesis (increase in blood volume) and the overall gradual increase in testosterone levels that more closely mimic normal hormonal function. This, by extension, keeps estradiol levels from skyrocketing and requires an aromatase inhibitor like clomid to prevent gynecomastia (ie “bitch tits”).
Non Medical Therapies
In addition to testosterone replacement therapy, there are also several lifestyle changes that can help improve testosterone levels. These may include maintaining a healthy weight, engaging in regular exercise, reducing stress, and avoiding alcohol and tobacco. According to a study published in the Journal of the American Medical Association, maintaining a healthy weight and engaging in regular exercise can significantly increase testosterone levels in most cases.
Based on this study and more compelling evidence, I created a 5 step, 90 day BE.A.S.T. Body Blueprint program designed to improve testosterone levels, naturally. Each step addresses a major pillar of hormonal health. The goal is to provide not only a great workout plan but a customized meal plan that is non-restrictive, a doctor inspired mobility plan to reduce chronic pain and a Navy SEAL approved sleep hygiene plan to get your testosterone moving in the right direction so that you can lose weight and feel great again.
Conclusion
Low testosterone is a growing concern for military veterans, but with proper treatment and care, it is a condition that can be managed and controlled. If you are experiencing symptoms of low testosterone, it is important to talk to your doctor and get a proper diagnosis. With the right support and care, you can reclaim your health, vitality, and continue to live life to the fullest.
In conclusion, low testosterone is a significant problem that affects many military veterans. The exact reason for the increased incidence of low testosterone among veterans is still unknown, but it is believed to be linked to stress, exposure to toxins, and physical trauma. With a proper diagnosis and the right treatment, low testosterone is a condition that can be effectively managed and controlled. If you are a military veteran and are experiencing symptoms of low testosterone, it is essential to talk to your doctor and get a proper diagnosis.
Talk to your doctor if Natesto® might be the right choice for you.
Train Hard, Fight Easy
Dave
Common Questions About Low Testosterone in Veterans
Understanding low testosterone is crucial for veterans. Here are some frequently asked questions and their answers to help you navigate this condition.
What are the symptoms of low testosterone?
How is low testosterone diagnosed?
What treatment options are available for low testosterone?
Are there any risks associated with testosterone replacement therapy?
Can lifestyle changes help manage low testosterone?
Is low testosterone common among veterans?
Take Action for Your Health
If you suspect you have low testosterone, don’t wait. Seek medical advice today. Visit our resources page for veterans to find support and treatment options tailored to your needs.

